Abstract
AIMs:
Primary immune thrombocytopenia (ITP) is a common bleeding disorder characterized by low platelet counts, which could cause serious bleeding. One hallmark of ITP is the production of platelet-specific autoantibodies, resulting in accelerated platelet destruction and impaired platelet production. The anti-platelet antibodies normally react with components of platelet glycoproteins (GPs), which are rich in negatively charged amino acids. However, it is not clear how these autoantibodies are generated in ITP patients. The aim of this study is to investigate the status of B cell central tolerance in ITP.
Methods:
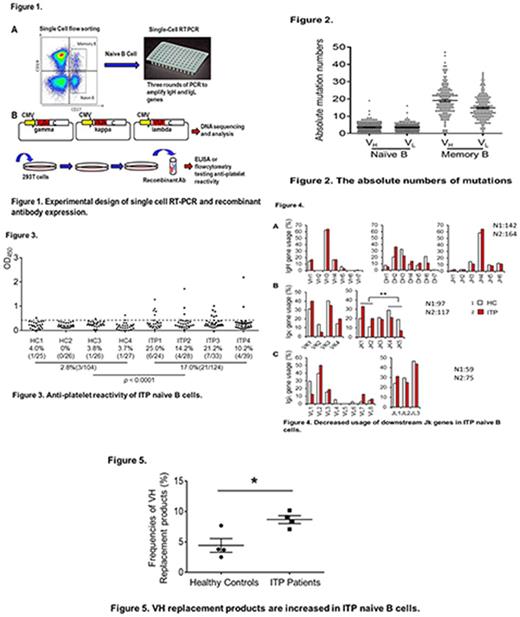
To gain an insight into the early B cell tolerance in ITP, we investigated the B cell receptor (BCR) specificity and immunoglobulin genes of naïve B cells in ITP patients. Naïve B cells were sorted and distributed into 96-well PCR plates at one single cell per well by single cell flow sorting. Paired immunoglobulin heave (IgH) and light (IgL) chain genes were amplified by reverse transcription PCR from single naïve B cells. The correct PCR products were subcloned into corresponding vectors and sequenced. Matched IgH and IgL genes from the same B cell were co-transfected into HEK293 cells to express recombinant antibodies (Fig. 1). The reactivity of these antibodies against platelet antigens was determined by ELISA, immunofluorescence assays, and flow cytometry. Ig gene sequence features were analyzed by programs including IMGT, IgBLAST, and VHRFA-1.
Results:
So far, 228 recombinant antibodies were expressed derived from naïve B cells in 4 ITP patients and 4 healthy controls. The absolute numbers of somatic mutations (nucleotide exchanges compared with germ line) of VH and VL between naïve B cells and peripheral memory B cells revealed significant difference (5.1 and 4.4 v.s. 19.0 and 14.8, p < 0.05 in both comparisons), indicating that the sorted cells were actually naive B cells (Fig. 2). ELISA assay showed that 17.0% (21/124) of the ITP-derived naïve B cells were platelet-reactive, in contrast to the 2.8% (3/104) in healthy donor-derived naïve B cells (Fig. 3), suggesting a defective B cell tolerance in the early developing stage. The anti-platelet reactivity was also confirmed by immunofluorescence assays and flow cytometry. Sequence analysis revealed that positively charged amino acids were highly enriched in the complementarity determining region 3 (CDR3) of the anti-platelet antibodies, which possibly generates the potential to interact with the negatively charged glycoproteins. The IgL genes derived from ITP patients preferentially used upstream JΚ segments (25.7% v.s. 49.1 %, p < 0.01) compared with healthy controls, indicating an insufficient IgL receptor editing in ITP patients (Fig. 4). In addition, the frequencies of VH replacement products in ITP were elevated in IgH genes from ITP patients (8.6% v.s. 4.4%, p < 0.05) compared to healthy controls (Fig. 5).
Conclusion:
In summary, this study provides evidence of defective early B cell tolerance and accumulation of anti-platelet naïve B cells in patients with ITP. This defect might be a result of insufficient receptor editing in IgL as well as excessive VH replacement in IgH.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal